Pursuing equity in public health emergency preparedness and response is critical to ensuring health departments meet the needs of vulnerable populations. This involves justly distributing resources, addressing unique needs, and acknowledging the social determinants of health to create inclusive preparedness and response plans and practices. However, several challenges often make it harder for health departments to effectively implement these equitable practices. These include the lack of appropriate disability data, workforce underrepresentation, and a lack of attention to equity goals during crisis situations. Recognizing these factors is a vital step toward addressing them and fostering a more inclusive and effective public health infrastructure.
By exchanging experiences and fostering mutual learning, state and territorial health departments can turn challenges into opportunities for advancing equity in their communities.
Common contributing factors to these challenges include:
not_accessible
Lack of appropriate disability and race/ethnicity data: There is a lack of enforcement and accountability to ensure health organizations and federal agencies are including required demographic survey questions in their data collection.
settings_ethernet
Lack of infrastructure for special populations: Many jurisdictions don't have the infrastructure to collect data that would indicate a need to prioritize the health and safety of those regarded as "special populations," such as pregnant and postpartum women and infants and children and youth with special healthcare needs.
psychology
Inadequate understanding of equity issues: There is a significant lack of data to help health departments understand and address equity issues in public health.
settings_accessibility
Lack of Workforce representation: Often, the public health workforce doesn’t demographically represent the populations it serves.
crisis_alert
Overlooking equity goals in crisis mode: All health departments have equity goals, but these often get forgotten during moments of crisis. Public health staff need intentional training on how to operationalize anti-oppressive and anti-racist practices during emergencies.
query_stats
Need for oversampling: There is an almost universal need for oversampling to ensure there's enough data about populations experiencing significant outcome disparities for health departments to use to appropriately establish and fund programs.
psychology
Lack of urgency around data disaggregation: There is not enough urgency around disaggregating data in order to tell more complete stories about populations experiencing significant outcome disparities.
This section highlights a successful and innovative solution your peers implemented to address challenges with inequities in public health preparedness and response. This story presents the factors to catalyze innovation, the existing policies or funding mechanisms that facilitated action, the potential barriers the agency faced, the collaborations and partnerships the agency leveraged, and tips for implementing and/or scaling the solution.
Innovative Strides Toward Health Equity: State-Led Initiatives in Emergency Preparedness
Introduction
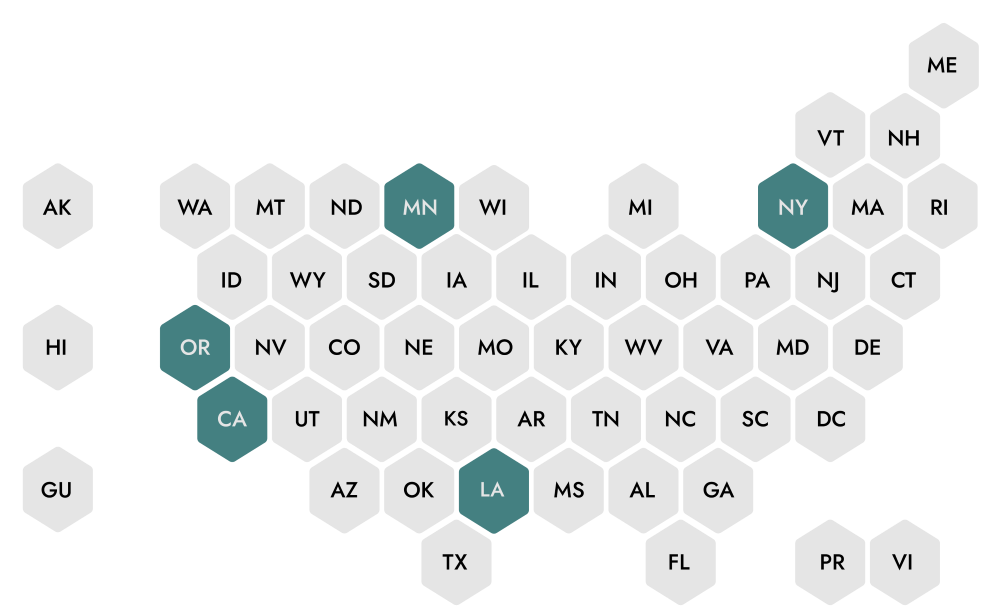
During public health emergencies, health departments must prioritize ensuring equal access to health resources and addressing health disparities. Multiple states have taken significant steps to promote inclusion and equity in emergency preparedness, showcasing unique approaches to alleviating disparities and driving health equity efforts forward. California, New York, Oregon, Minnesota, and Louisiana stand out for their commitment to equal access and innovative strategies to address health inequities.
Vulnerable populations are disproportionately impacted by disasters, and climate change further exacerbates the frequency and severity of these impacts. California's Office of Health Equity (OHE) has emerged as a leader in promoting health equity as part of the statewide response to climate change. To enhance the state’s emergency planning and response capacity, OHE’s Climate Change and Health Equity Section launched the CalBRACE project in 2016. CalBRACE primarily helps local agencies, community partners, and tribal organizations develop policies, data collection methods, and strategies to incorporate climate adaptation and health equity considerations into their operations. CalBRACE also maintains a hub of web-based tools and resources for adaptation planning, consulting and engagement resources, risk and burden assessments, and implementing and evaluating adaptation initiatives.

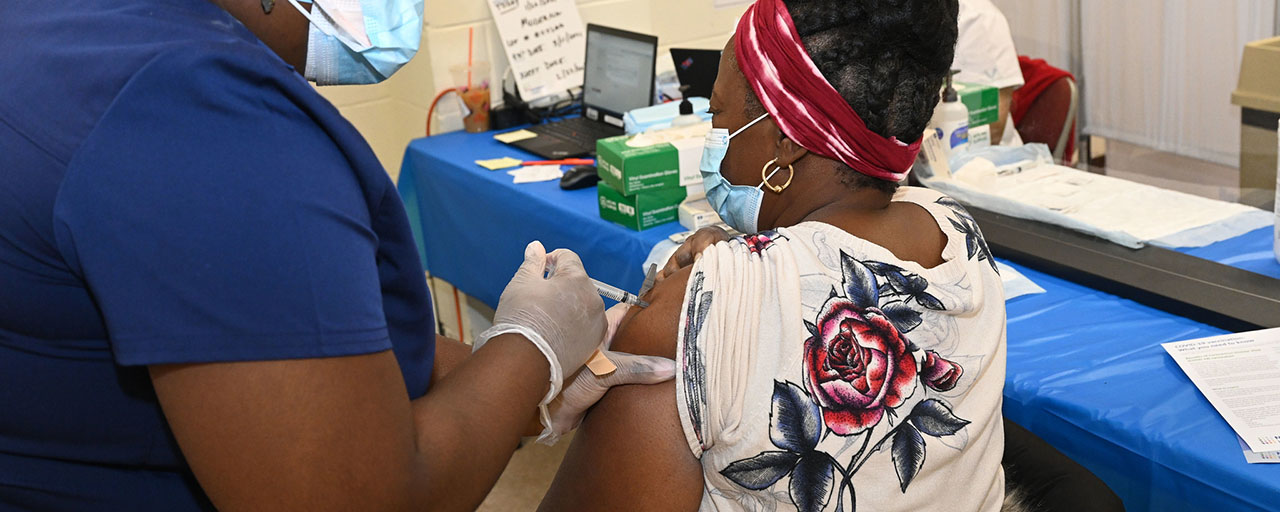
In New York, the COVID-19 pandemic revealed the driving forces behind health disparities in communities of color. The history of exploitation and mistreatment of minority patients by medical professionals had led to deep mistrust and vaccine hesitancy. In response, the state formed the COVID-19 Vaccine Equity Task Force, which aimed to ensure fair and equitable vaccine distribution and promote community confidence in public health measures. The task force worked closely with local organizations to launch pop-up vaccination sites across the state. Collaborating with community organizations has also been key to combating misinformation and providing culturally-sensitive education about the benefits of vaccination.
The Oregon Health Authority (OHA), which has had a longstanding focus on health equity, employed two key strategies that can serve as practical examples for other states seeking to enhance their health equity efforts. In 2019, OHA’s Equity and Inclusion Division partnered with community representatives across the state and the Oregon Health Policy Board’s Health Equity Committee to establish intentional and operationalizable definitions of “health equity” and other key terms used to describe equity efforts. Involving communities in this first step helped to empower community members, encourage cross-stakeholder collaboration, and form authentic relationships and clear communication pathways. In 2021, OHA leveraged the relationships built through its first strategic action to develop a comprehensive equity advancement plan, which focused on improving the mechanisms for robust internal and external coordination and community impact. As part of this plan, Oregon adopted the strategic goal to end health inequities in the state by 2030, a goal informed by OHA’s continuous community engagement. During the state’s COVID-19 response, OHA used the plan as guidance for its emergency funding proposal to infuse the most vulnerable tribal communities across the state with food supplies, medical resources, and business assistance, proving the value of intentional strategic planning for equity and inclusion.
The Minnesota Department of Health (MDH) has developed a similar health equity and inclusion plan, emphasizing that health inequities are the main challenge facing state, local, and tribal health departments. As part of this plan, one of the department’s key strategies for advancing health equity is to listen authentically to and partner with communities. The MDH Community Engagement Unit focuses on forming engagement practices that build on assets and drive solutions created in partnership with communities. To address the root causes of inequity, the unit helps public health organizations transform their organizational operations, policies, budgets, hiring practices, and data collection methods to emphasize equity and inclusion. In 2017, MDH launched its Health Equity Learning Community in six local jurisdictions, providing a space where health departments can share success stories and lessons learned so that other organizations can replicate and scale their work.
Lastly, Louisiana’s Bureau of Family Health, in partnership with the Louisiana Department of Health (LDH), has showcased an innovative, data-driven approach to addressing health inequities. In 2016, the Bureau of Family Health brought together staff and community partners as the Health Equity Action Team to promote health equity within its culture, workflow, and services. The team’s 2017-2019 action plan explored the impact of systemic oppression and institutionalized racism on the health of Louisiana’s families. In response to these findings, the LDH Office of Community Partnerships and Health Equity launched its Health Equity Plan and Framework, which requires each LDH office to establish its own action team. Among these teams, the work of the Data Collection, Analysis, and Distribution Team stands out for its unique focus on advancing equity through organizational changes. The team prioritizes equity during regular data analysis to reduce bias and limit unintended consequences, and has developed equity-related professional competencies for the Data-to-Action team staff.
Policies and Funding
Adopting such initiatives requires policy changes that prioritize health equity, as well as sustainable funding adjustments to accommodate and bolster these new programs. Various federal agencies have dedicated funding pools to health equity activities. CDC offers several grant programs for health equity initiatives, including the Racial and Ethnic Approaches to Community Health program. HHS’ Office of Minority Health also provides grants to support agencies working to eliminate health disparities among racial and ethnic minority populations, including tribal communities. Health departments should also consider nonprofit hospitals, private hospital systems, and public community foundations with a special interest in health equity investments as potential funding partners. National and regional foundations and corporate philanthropies, such as the Robert Wood Johnson Foundation, can also help with technical assistance and sustainability efforts.
Challenges and Barriers
- Securing consistent funding: Policy advocacy and partnerships can help procure flexible and sustainable funding. Health departments should keep in mind the timing of funding when deciding on the scope of their equity programs.
- Complexity of systemic issues: By nature, health equity programs focus on complex and systemic issues, often with intersecting and deep-rooted challenges. Progress may occur over long periods and may be nonlinear, so health departments should carefully balance short- and long-term goals.
- Securing stakeholder buy-in: Health departments should seek to generate buy-in from government stakeholders, businesses, and community members. Some organizations may also need to transform their own organizational culture before they are ready to lead and implement health equity programs.
- Building authentic community relationships: Community engagement is central to a successful health equity program. It is essential that such programs center the voices, experiences, wisdom, and goals of community members in their work. Programs should consider how community participation is affected by lack of access to resources, mistrust resulting from historical mistreatment, and unbalanced power dynamics between communities and institutions.
- Framing health equity issues and messaging: Terms related to health equity may sometimes carry controversial connotations. Programs should carefully consider the kind of messaging and language they use to describe issues, data, and initiatives, in collaboration with their communities. Appropriate messaging can help develop a shared understanding of a program’s goals and increase stakeholder buy-in.
Collaborations and Partnerships
Collaboration and partnerships play vital roles in these initiatives. By working closely with local agencies, community partners, and tribal organizations, states can better integrate health equity considerations into local operations. Hospitals and health systems, community-based social service providers, business leaders, and faith-based organizations, among others, can be essential to building capacity and encouraging community member participation.
In addition, sustained and enthusiastic buy-in from policymakers is crucial to securing funding and encouraging high-level readiness for change.
Tips for Scaling
For health agencies contemplating similar initiatives, the following tips may be helpful:
- Advocate for policy changes that prioritize health equity.
- Establish strong partnerships with local and tribal organizations.
- Plan in advance to intentionally gather and incorporate community feedback into evolving programs.
- Transform agency organizational practices to include health equity considerations as a model for other organizations.
- Secure reliable funding sources.
- Ensure transparent and efficient data management processes.
APPLYING THIS KNOWLEDGE TO INFECTIOUS DISEASE
Initiatives aimed at promoting health equity in emergency preparedness can significantly benefit infectious disease practice and policy in the following ways:
- Inclusive emergency preparedness: Including all populations in emergency preparedness plans ensures that the most vulnerable individuals are considered in disease prevention and response strategies.
- Data-driven equity efforts: Using data to drive health equity initiatives can help identify disease trends among different population groups, inform policy decisions, and ensure resources are allocated where they are most needed in infectious disease management.
- Community engagement: Engaging with local communities in health equity efforts ensures that the needs and perspectives of local communities are considered in disease prevention and response strategies.
- Policy advocacy: Advocacy is crucial in securing funding and support for health equity initiatives. Sustained advocacy is needed to secure resources and policy support for disease prevention and response efforts.
- Workforce representation: Having a workforce that represents the population it serves can bring a broader range of perspectives and experiences to an initiative, leading to more inclusive and effective disease prevention and response strategies.
- Addressing systemic issues: Addressing the complexity of systemic issues that contribute to health inequities is crucial. It underscores the need to tackle underlying systemic issues to effectively prevent and respond to infectious diseases among all population groups.
This section encompasses a collection of pertinent tools and resources, curated from ASTHO's Public Health Innovations Catalog and various other sources to help you navigate and comprehend the intricacies of this subject area. Garnering insights and experiences from your peers will enable you to start building solutions tailored to your health department.
Feeling inspired to address the unique challenges facing your department? With just one click, you can gain a better understanding of your department's specific gaps and craft a persuasive action plan to present to your leadership and partners.
or explore the other focus areas:
Workforce Training & Resources Data Systems & Management Equity
Email the preparedness team with questions or comments.