Sustaining DMI: Medicaid Advanced Planning Document Process
July 24, 2024
Why is the Advanced Planning Document process important?
Based on information from the Government Accountability Office (GAO), the Centers for Medicare & Medicaid Services (CMS), and the Federal Register, the Advanced Planning Document (APD) process is a procedure through which states develop a plan of action for their Medicaid information technology (Medicaid IT) projects. These plans are for designing, implementing, or operating Medicaid Enterprise Systems (MES) projects. State Medicaid agencies (SMAs) submit completed APDs to CMS—specifically a designated state officer in the Center for Medicaid and Children’s Health Insurance Program (CHIP) Services (CMCS) Data and Systems Group (DSG)—to request federal financial participation for their activities. The state officer reviews APDs to assess whether states’ requests for federal financial participation for designing, developing, implementing, or maintaining MES activities contribute to the economic and efficient operation of Medicaid and meet specific technical and operational criteria defined in statute, regulation, or sub-regulatory guidance. A state that receives federal financial participation can see increased access to stable federal funding to support MES activities. In addition, APDs are used to monitor a state’s project performance and outcomes.
What are the three types of APDs?
There are three types of APDs: Planning, Implementation, and Operational (Table 1).
Table 1. Types of Advanced Planning Documents
| Type of ADP | Description | Example* | More Information |
|---|---|---|---|
| Planning |
|
An update to a Planning APD developed by Florida’s Agency for Health Care Administration. | |
| Implementation |
|
SMAs used this implementation APD template to request funding under the Electronic Health Records Incentive Program. |
|
| Operational |
|
Operational APD developed by the Office of Child Support Services. |
* C.F.R. identifies the components of an APD submission. The templates and styles may vary. All APDs can be updated. For example, the acronym for an updated Implementation Advanced Planning Document is “IAPD-U.”
What are the major steps for states in the APD process?
To request enhanced federal funding for MES, SMAs must complete the APD template that aligns with where they are in the development of their project (for example, design or maintenance) and submit it to the designated CMCS DSG state officer. The APD process contains five major steps and can take many months to complete: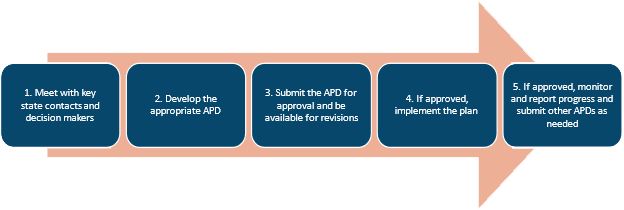
-
Meet with key state contacts and decision-makers.
Based on information from the Public Health Informatics Institute’s information and tip sheets, before developing the APD, the SMA should identify and engage key state contacts and decision makers to solicit their input about the proposed project and secure their and their staff’s collaboration to complete and submit the APD to the CMCS DSG state officer. The state health agency (SHA) should work closely with the SMA during this process to ensure that they provide needed support to the SMA. For example, the SHA may gather information for the SMA to include in the APD or advise on how to complete particular sections of the APD. During this process, the SMA and SHA should consult with their respective agency leadership to discuss the type of technological solutions Public Health maintains, Public Health’s relationship with the state Medicaid program, and the opportunity to align systems to reduce overall state costs and improve state efficiency through the APD process. The SMA and SHA should also engage the MES lead, who can offer critical information about current MES components and component certification needed to complete the APD. In addition, GAO recommends states involve their chief information official in overseeing Medicaid IT projects because they can play a critical role in decision making related to IT budgets, management, and oversight. Next, the SMA and SHA should engage the CMCS DSG state officer to develop a strong understanding of how the APD can support the Medicaid program and serve a public health interest. Coordinating with the state project management office can help integrate the diverse parties and processes needed to develop and submit the APD for approval. It can also help ensure that states develop a comprehensive and flexible timeline for the APD process, stay aware of approaching deadlines, and meet ad hoc requirements.
-
Develop the appropriate APD.
Next, based on 45 C.F.R. § 95.610(c), the SMA and SHA should identify which of the three types of APDs to submit to the CMCS DSG state officer. Planning APDs are recommended for large and complex projects, such as statewide projects. However, if a state can identify a clear and easy pathway to integrate a public health information technology system with a current MES procurement or development phase, it can forgo developing a Planning APD and directly develop or update an existing Implementation APD. For example, if a state is looking to integrate its counties’ public health data into its MES at once, it should develop a Planning APD as the project is large and affects all counties in the state. However, if a state already has most of its counties’ public health data in its MES but is looking to add a single county’s data to its MES using the same process it previously and successfully used to add the other counties’ data, it may not need to submit a Planning APD. If a state has already successfully integrated its counties’ public health data into its MES and is looking to make major technology upgrades and improvements, it should submit an Operational APD. Regardless of the type of APD the state submits, the SMA and SHA should work together to ensure the request meets the Conditions for Enhanced Funding (see separate document Conditions for Enhanced Funding: The Basics).
-
Submit the APD for approval and be available for revisions.
Based on information from CMS, GAO, and the Office of Child Support and Enforcement, the state should then submit the APD to the designated CMCS DSG state officer. The SMA and SHA should plan to receive questions and revision requests from the CMCS DSG state officer and ensure that the state has staff capacity to answer questions and revise and resubmit. Approval conditions can be found at 45 C.F.R. § 307.15, but approval criteria might vary by Medicaid IT project and other factors.
-
If approved, implement the plan.
Next, the state can carry out the plan described in its Planning and Implementation APDs. After the Medicaid IT project has been operating for at least six months, states can request system certification from CMS. According to CMS, certification is required to receive the enhanced 75 percent federal financial participation for operations. The certification process includes states submitting to CMS an intake form, a certification request letter, and supplemental materials with information on its system. CMS may then start its review to assess whether the state’s system meets certification requirements.
-
If approved, monitor and report progress and submit other APDs as needed.
Based on 45 C.F.R. § 95.610(c) and 45 C.F.R. § Part 95 Subpart F and information from CMS, CMCS, Office of Child Support and Enforcement, as the state continues with its Medicaid IT project, it should adhere to monitoring and reporting requirements for enhanced federal funding. It also should submit annual APDs as required. If the state wants to make any major changes to the Medicaid IT project in concept, scope, cost allocation approach, timeline, and other key areas, it must develop and submit an as-needed APD. An as-needed APD is due no later than 60 days after the occurrence of the change.
State examples: Medicaid Enterprise System projects
Based on information from Alvarez & Marsel, state MES projects will vary based on factors such as the maturity of a state’s technology infrastructure, its specific data needs, and its available resources. As such, projects to design, implement, or operate MES can range in size, complexity, and timeline. For example, the Alabama MES Modernization Program, the Wyoming Integrated Next Generation System Project, and the Florida Health Care Connections project all seek to transform their singular Medicaid Management Information Systems (MMIS) into modular, multi-vendor MES, but differ in approach. In addition, Arizonia and Hawaii are collaborating to modernize their shared MES.
For more information on state MES projects, see the Medicaid Enterprise System Solution/Module Contract Status Report. This webpage lists states’ MMIS and Eligibility and Enrollment contract information for their MES projects. It also lists contact information for state officers to reach out to learn more about states’ MES projects.