Opioid Preparedness: Disruptions in Access to Prescription Opioids
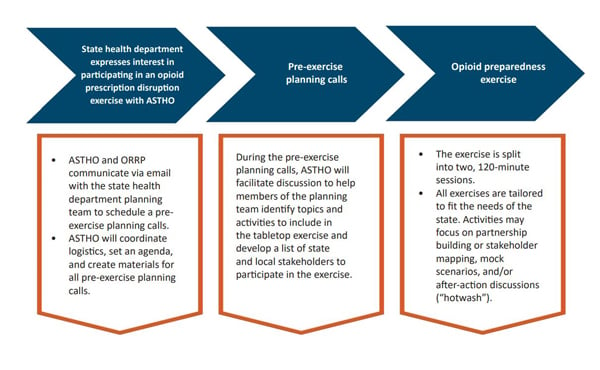
ASTHO, with support and collaboration from CDC’s Opioid Rapid Response Program (ORRP), helps its members by conducting scenario-based preparedness exercises with health agency staff and diverse partners to support planning for and responding to disruptions in access to opioid prescriptions or medications for opioid use disorder (MOUD). ASTHO and ORRP work together to incorporate lessons learned from real actions and state responses into the practice exercises to ensure they represent realistic scenarios.
What are Disruptions?
Overdoses involving prescription opioids, heroin, and synthetic opioids have increased nearly sixfold since 1999. In 2020, the United States saw the greatest number of overdose deaths ever recorded as the social and economic conditions associated with the COVID-19 pandemic converged.
A disruption is any event that halts the ability of a patient to access opioid prescriptions or MOUD, including a provider’s death or retirement or a regulatory/licensing action against a prescriber. These events can be especially dangerous for displaced patients, who face increased risk of negative physical and mental health effects including feelings of abandonment, depression, and symptoms of withdrawal. In the absence of continued care, patients experiencing untreated pain or withdrawal may turn to the illicit drug market, putting them at increased risk for overdose. Furthermore, with the changing landscape in the illicit market, disruptions have become a more urgent; pressing issues such as fentanyl and counterfeit prescription pills have created a more deadly supply.
What is the Opioid Rapid Response Program?
The Opioid Rapid Response Program (ORRP) is an interagency, coordinated federal effort to help mitigate overdose risks among patients who lose access to a prescriber of opioids, MOUD, or other controlled substances (e.g., benzodiazepines). ORRP is overseen by the Office of the Assistant Secretary for Health (OASH) and is managed by CDC in partnership with HHS’s Office of the Inspector General.
Opioid Preparedness Exercises
ASTHO’s preparedness tabletop exercises will aim to provide information and build knowledge about opioid closure events, facilitate important planning discussions among key state agencies and organizations, and provide a structure for developing and/or refining a written response protocol. These exercises are based on the Homeland Security Exercise and Evaluation Program (HSEEP) tabletop exercise model—a discussion-based scenario that facilitates conceptual understanding, identifies strengths and areas for improvement, and/or achieves changes in perceptions about plans, policies, or procedures.
The time commitment is two hours per session, for a total of four hours.
Exercise participants have included state and local health department and behavioral health agency staff, peer recovery specialists, first responders, physicians, linkage-to-care coordinators, drug overdose prevention specialists, hospital systems, private payers and Medicaid, primary care associations, and community health center associations, among others.
Opioid Preparedness Resources
Exercise Overview
The summary document provides an overview of ASTHO’s opioid preparedness exercise and outlines what participants can expect when attending a session.
Guidebook

The guidebook focuses on how state health agencies can prepare for and respond to disruptions in patient access to opioid prescriptions MOUD. This resource also explores why disruptions occur and the possible risks to patients, how state response plans may look, and includes helpful information and examples that support state protocol development.
Response Protocol Template

This modifiable tool serves as a template for states to adapt and reference when developing a protocol for planning for and responding to disruptions in access to opioid and other controlled substance prescriptions due to a law enforcement action against a healthcare provider.
Opioid Preparedness Exercise in a Box

This module houses all the materials that a state or territory would need to plan and facilitate an exercise to develop, test, and/or enhance a state response protocol for responding to disruptions in access to opioid prescriptions or medications for opioid use disorder.
Trusted Contacts Training Modules
Three on-demand training modules detail what it means to be a state trusted contact for CDC’s Opioid Rapid Response Program and provide essential background for state trusted contacts to better prepare for and respond to disruptions in access to opioid prescriptions.
Reduce Stigma to Improve Care for Patients Taking Long-Term Opioid Therapy Resources
Long-term opioid therapy (LTOT) is often prescribed for chronic pain when other options have failed. However, due to the history of widespread opioid overprescription and the current overdose crisis, LTOT is associated with negative perceptions. This stigma poses a barrier to care continuity for these patients, which is particularly concerning, as abruptly discontinuing such medication can lead to adverse health effects due to physical dependency. These resources assist healthcare workers and state health departments in addressing and mitigating stigma affecting patients on LTOT.
How Healthcare Providers Can Reduce Stigma to Improve Care for Patients Taking Long-Term Opioid Therapy
This report aims to increase awareness among healthcare providers about the stigma surrounding LTOT and emphasizes the importance of addressing it to ensure proper care for individuals dependent on these medications.
How State Health Departments Can Reduce Stigma to Improve Care for Patients Taking Long-Term Opioid Therapy
This resource aims to assist state and territorial health departments in mitigating stigma affecting patients already on LTOT for chronic pain, emphasizing the importance of care continuity to prevent serious health risks associated with abrupt medication discontinuation.
Learning Community Sessions
Session 1: Risk Assessment
Session 2: Risk Mitigation Strategies
Session 3: Establishing Continuity of Care
Session 4: Building Partnerships with Payers
The development of this product is supported by the Center for State, for State, Tribal, Local, and Territorial Support (CSTLTS) at the Centers for Disease Control and Prevention (CDC) of the U.S. Department of Health and Human Services (HHS) through the cooperative agreement CDC-RFA-OT18-1802.