Member Spotlight: Tomás J. Aragón
October 14, 2021 | Andrew Tucker
Tomás Aragón, MD, DrPH serves as the director of the California Department of Public Health and the State Public Health Officer, since January 4, 2021. Prior to coming to CDPH, he was the health officer for the City and County of San Francisco and director of the public health division. In this post we discuss how COVID has impacted the Latino community.
What are the biggest public health challenges facing the Hispanic and Latino community in your jurisdiction? What shifts must occur to tackle these issues?
Many people put Latinos in a single bucket, but the Latino population is very complex. So it’s both difficult and limiting to discuss it as a single community. When considering social determinants of health such as poverty, education, racism, and environment, a disproportionate number of Latinos live in disadvantaged communities. As such, they have less access to high-quality health care, safe and clean neighborhoods, healthy food and other factors, all of which lead to adverse health outcomes. These disparities can be further perpetuated when place, and immigration status is taken into consideration.
Leading Causes of Death, Hospitalization, and ED Visits for Latino Race/Ethnicity in CALIFORNIA: 2018-2020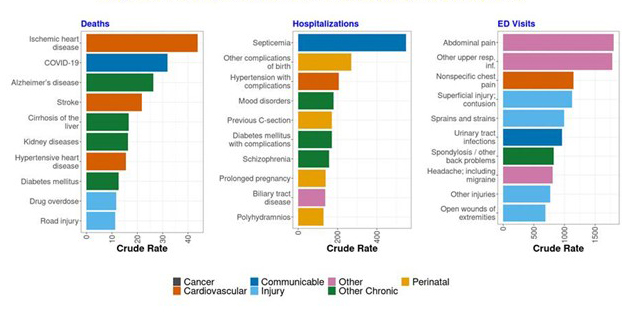
Working with the Latino community is so much more than Spanish language transition. There are indigenous dialects, different populations, and the best ways to reach those populations aren’t the same. We need more media outreach and focus groups to better understand the complexity of communities—and not just Latinos. Once we have a better understanding, we can develop the best messaging, channels, and messengers.
Hispanic persons are 1.9 times more likely to contract COVID-19 than non-Hispanic White persons, and 2.8 times more likely to be hospitalized from the virus. What do you see as the role of state health officials in addressing these disparities?
Pre-COVID-19, Latinos were among the healthiest population in the Southwest despite having more socioeconomic, health, and immigration barriers; some people call this the “Hispanic paradox.” When COVID hit, Latinos were in a very vulnerable position. The things that kept Latino families connected—the social cohesion of large families—also put them at risk for COVID transmission. Infections were happening in essential workers, a group in which Latinos are overrepresented. But they had to go to work and use public transportation. It led to more crowding and exposure. Their jobs don’t always provide health insurance or paid sick leave.
We need to focus on interrupting transmission no matter where it is. If there’s more transmission happening, we know who’s suffering the most, and who’s getting exposed, infected, and bringing it home. They’re working in restaurants, working in the kitchens, and hotels.
The COVID-19 vaccination campaign has underscored the importance of building relationships with members of racial and ethnic minority communities. How we can we build a more inclusive public health response?
Building relationships and trust takes years. Prior to the pandemic, I was at the San Francisco Department of Public Health. Because African Americans had poorest health status, we were already working with churches to address food insecurity, the basis of so many health issues. In the process of meeting food insecurity needs, we learned more about the community and their concerns about violence, housing, and other social problems. When COVID-19 hit, we had already built a network of trusted communication with the African American Community. That process took much longer with the Latino community. We didn’t have the depth of relationships that we did with the African American community. To build that trust is hard to do that at a state level and must involve counties and cities.
Public health organizations won’t be successful in the community without transforming their own institution. Moreover, racial equity work—the transformation of self, team, and organization—needs to be done in partnership with communities. Public health organizations need to recruit, hire, and retain staff with proper public health competencies to engage with communities of color. An overall investment needs to be made prior to rapid, crisis and emergency issues—workforce is key to ensure racial and ethnic communities are properly reached, engaged, and served.
What is being done—and what must we do better—to strengthen Latino and Hispanic representation in the public health workforce?
In California, Latinos are underrepresented in all health fields. While making up 39% of California’s population (and 50% in Los Angeles), there is woeful representation within health professions, and that’s true in medicine and public health leadership. A lot of work needs to be done in recruitment and retention. At the state level, our office of health equity is planning an initiative called the future of public health. Part of this is going to be recruitment and retention, including a public health service corps to train people. That will take some time, and we must establish career pathways for Latinos. But public health can’t do it by itself. It’s an all-government response.