Forward Focus: The Urgent Need to Address Rising Cases of Viral Hepatitis
December 15, 2021 | Shalini Nair
 In the backdrop of the COVID-19 pandemic, cases of viral hepatitis continue to rise at alarming rates across the United States. Data from CDC highlights a 133% rise in cases of acute hepatitis C infection from 2012-2019 and new case counts four times higher than those seen a decade ago. Additionally, although the United States met annual targets for reduction in cases and deaths associated with chronic hepatitis B, continued efforts to increase awareness of testing and linkage to care remain necessary.
In the backdrop of the COVID-19 pandemic, cases of viral hepatitis continue to rise at alarming rates across the United States. Data from CDC highlights a 133% rise in cases of acute hepatitis C infection from 2012-2019 and new case counts four times higher than those seen a decade ago. Additionally, although the United States met annual targets for reduction in cases and deaths associated with chronic hepatitis B, continued efforts to increase awareness of testing and linkage to care remain necessary.
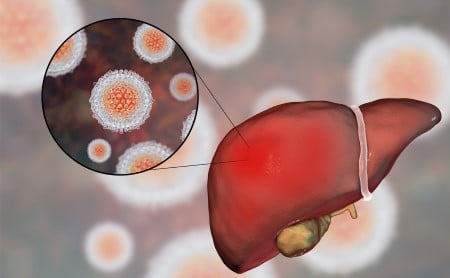
Chronic hepatitis B or C infection can result in potentially life-threatening health outcomes, including cirrhosis and liver cancer. Despite this, upwards of 50% of individuals living with chronic hepatitis B or C infection may be unaware of their status. Additionally, chronic viral hepatitis contributes significantly to the nation’s healthcare expenditures, with total costs for hepatitis C alone estimated to be upwards of $6 billion and Medicare treatment costs expected to top $28 billion for the period ranging from 2017-2026.
Major increases in both forms of viral hepatitis tend to cluster in alignment with jurisdictions and age groups most affected by the injection drug use crisis. People who use drugs are at increased risk of bloodborne exposure to hepatitis B and C, with approximately 35% of hepatitis B and 67% of hepatitis C cases with available risk information reporting intravenous drug use.
This phenomenon, commonly referred to as a syndemic, highlights the interplay between viral hepatitis and other conditions including STIs, HIV, mental health, and substance use disorders. The detrimental consequences of this synergism are further exacerbated by the COVID-19 pandemic’s impact on screening and provision of services.
State and territorial health officials play a crucial role in the planning and implementation of viral hepatitis elimination activities. In 2018, ASTHO, with support from CDC, issued awards to seven state health agencies (Indiana, Iowa, Louisiana, Pennsylvania, Rhode Island, Virginia, and Washington state) to implement demonstration projects addressing hepatitis B and/or C. Building on these experiences, ASTHO released a report highlighting key approaches and resulting outcomes of these initiatives.
Based on this report and additional insight from the Viral Hepatitis National Strategic Plan, here are four ways that jurisdictions can address common barriers to elimination planning:
- Bolster Surveillance and Improve Data Usage
Capacity to collect viral hepatitis surveillance data remains limited and often lacks integration across program areas and systems. National decision-making based on incidence, prevalence, or epidemiological distribution of viral hepatitis relies on estimates, as public health program capacity remains insufficient to detect and report all cases to CDC.
Prevention efforts may be missing valuable opportunities to identify and link individuals living with hepatitis to care. Leveraging data sources including health information exchanges or individual patient records can help identify gaps in reporting or progression through the care cascade. Improved data access will allow for increased efficiency and rapid translation of findings into public health and clinical practice interventions targeted towards affected populations.
[ASTHO’s support has been] instrumental in supporting [a collaboration with] the Rhode Island Department of Corrections (RIDOC) to increase screening and treatment of their inmate population. RIDOC used the funding to establish an HCV Medical Committee and expand their electronic medical records, patient tracking tools, and referral systems for inmates released into the community for follow up care and services.”
- Thomas Bertrand, Chief of the Center for HIV, Hepatitis, STD, and TB Epidemiology at the Rhode Island Department of Health
- Increase Access to Services for High-Risk Populations
Given the syndemic nature of viral hepatitis, expanding access to testing and care in non-traditional settings may help increase the number of infected individuals who are aware of their status and prevent further transmission or disease progression. Multi-stakeholder partnerships offer unique opportunities to reduce silos in viral hepatitis prevention and treatment.
Other effective approaches may involve integrating hepatitis services at substance use disorder treatment centers and syringe service programs, or in non-clinical settings such as homeless shelters.
- Raise Awareness of Hepatitis Testing and Treatment
Public awareness of viral hepatitis is critical to increasing rates of screening, diagnosis, treatment, and—in cases of hepatitis C—cure. Many infected individuals do not present with any symptoms, prolonging the time to diagnosis. CDC is committed to promoting awareness of viral hepatitis and supports many annual observances, including Hepatitis Awareness Month and World Hepatitis Day. At the state level, jurisdictions may seek to capitalize on media outlets—including radio, print, television, and social media—to disseminate targeted campaigns encouraging individuals to get tested and seek care for hepatitis B or C.
ASTHO funding allowed Washington state to apply this strategy by “…focusing on three critical areas, which included: strengthening surveillance through the development of a state care cascade in partnership with the Center for Disease Analysis, scaling up provider proficiency in testing and treating hepatitis C through a telemedicine model, and increasing hepatitis C testing and treatment referrals among people who use drugs.”
- Jon Stockton, Washington State Department of Health, Adult Viral Hepatitis Prevention Coordinator
- Improve Healthcare Provider Capacity
To meet the goals of the National Strategic Plan, states should work to improve provider capacity for viral hepatitis treatment and care. This includes increasing knowledge of gender, age, or population-specific factors that may indicate screening or impact disease progression. Additionally, improving provider ability to identify, manage, and resolve barriers to care is essential.
Other strategies in this area may include offering clinician and staff trainings in virtual or in-person formats, or engaging providers in routine peer-to-peer learning sessions.
For additional details and to learn more about how states implemented the specific approaches mentioned above, we invite you to access the full report, State Strategies for Advancing Viral Hepatitis Elimination.