Best Practices for States to Identify and Address Breast Cancer Disparities
February 02, 2018 | Joshua Berry
In the United States, Black women are approximately 40 percent more likely to die of breast cancer than white women once diagnosed. “Disparities in breast cancer mortality represent a glaring injustice and require timely action,” says Marcus Plescia, MD, chief medical officer at ASTHO and former director of CDC’s Division of Cancer Prevention and Control. “State public health leaders are in a unique position to draw attention to this issue and champion evidence-based interventions to reduce inequities in follow-up care and treatment quality.”
To understand why the diagnosis is deadlier for some women, ASTHO was funded by CDC to create a breast cancer disparities learning community to help health departments in Arizona, Tennessee, and West Virginia identify and address the unique state and local disparities in breast cancer screening rates, the time it takes women to seek follow-up care after an abnormal test result, and cancer treatment quality. This work revealed many best practices, lessons learned, and resources to assist other health departments in addressing breast cancer disparities.
Best Practice #1: Use GIS Mapping to Generate Essential Data
Geographic information system (GIS) mapping is an important tool that public health professionals can use to identify disparities based on breast cancer and sociodemographic data at the county or local levels. Through the learning community, Esri, a GIS software and data analytics company, showed states how to perform spatial and epidemiological analyses with trainings, such as the “Bridging the Breast Cancer Divide” online course.
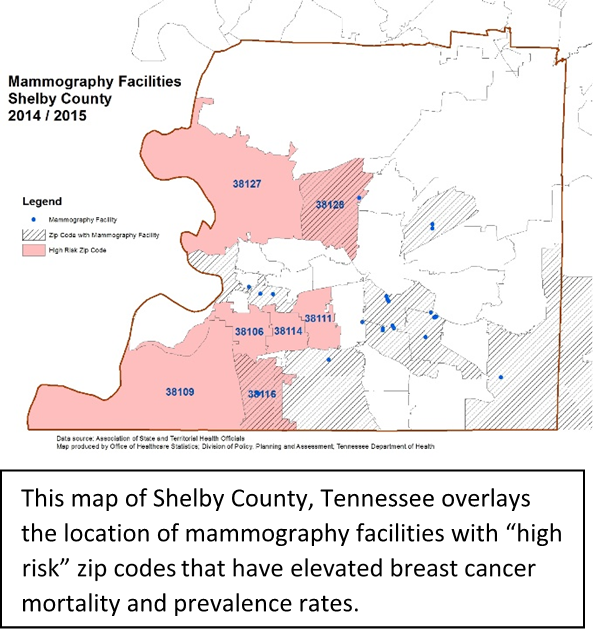 The Tennessee Department of Health team utilized GIS maps to display breast cancer rates and sociodemographic data in Shelby County and learned that this region, which includes Memphis, had some of the highest breast cancer mortality rates among black women in the entire state. As a first step to increase the number of women screened for breast cancer, Tennessee generated maps to pinpoint specific zip code areas where mobile mammography efforts could make the most impact. Other examples of GIS maps and state data reports can be found in the Tools section of ASTHO’s breast cancer online toolkit.
The Tennessee Department of Health team utilized GIS maps to display breast cancer rates and sociodemographic data in Shelby County and learned that this region, which includes Memphis, had some of the highest breast cancer mortality rates among black women in the entire state. As a first step to increase the number of women screened for breast cancer, Tennessee generated maps to pinpoint specific zip code areas where mobile mammography efforts could make the most impact. Other examples of GIS maps and state data reports can be found in the Tools section of ASTHO’s breast cancer online toolkit.
Best Practice #2: Understand How Sociodemographic Factors Affect Disparities
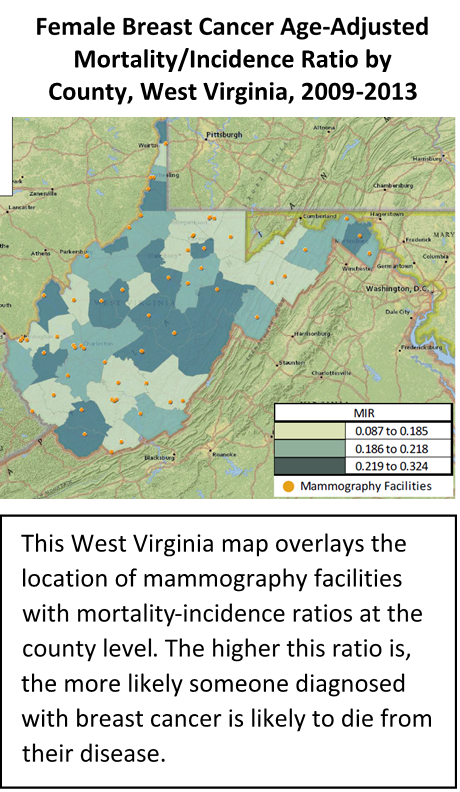 Disparities across various sociodemographic indicators can also influence mortality, including health insurance status, urban or rural residency, and proximity to the nearest mammography provider or accredited cancer treatment facility. The Approaches section of ASTHO’s online toolkit presents research on breast cancer disparities defined not only by race, but also factors such as geography, primary care access, and cultural characteristics and practices. West Virginia’s population is approximately 94 percent white, so the state focused its efforts on looking at indicators such as urban-rural classification, income level, and health insurance status. By broadening its scope, West Virginia successfully identified rural areas where mammography providers and accredited cancer treatment facilities were out of reach for many low-income residents, leading to the deployment and expansion of the Bonnie's Bus mobile mammography program.
Disparities across various sociodemographic indicators can also influence mortality, including health insurance status, urban or rural residency, and proximity to the nearest mammography provider or accredited cancer treatment facility. The Approaches section of ASTHO’s online toolkit presents research on breast cancer disparities defined not only by race, but also factors such as geography, primary care access, and cultural characteristics and practices. West Virginia’s population is approximately 94 percent white, so the state focused its efforts on looking at indicators such as urban-rural classification, income level, and health insurance status. By broadening its scope, West Virginia successfully identified rural areas where mammography providers and accredited cancer treatment facilities were out of reach for many low-income residents, leading to the deployment and expansion of the Bonnie's Bus mobile mammography program.
Best Practice #3: Promote Systems Change by Partnering Across Sectors
Partnering with diverse organizations and sectors is essential to sustaining the momentum and resources needed to address breast cancer disparities. Partners are instrumental in developing data-driven, targeted systems change interventions because they can provide access to important data and help analyze and disseminate key findings. State health departments may consider engaging healthcare providers, hospital systems, local clinics, insurance companies and other healthcare payers, researchers from academic institutions, and cancer prevention coalitions, such as local Susan G. Komen chapters. Many stakeholders are eager to get involved with efforts to address breast cancer disparities, but may not know how to contribute or fully understand the impact these disparities have on their communities. Having maps and data findings readily available and in a user-friendly format creates an easy opportunity for partners to contribute to reducing disparities within their existing roles. The Assessment section of ASTHO’s online toolkit lists the types of partners who contributed to the learning community and their respective roles within each state.
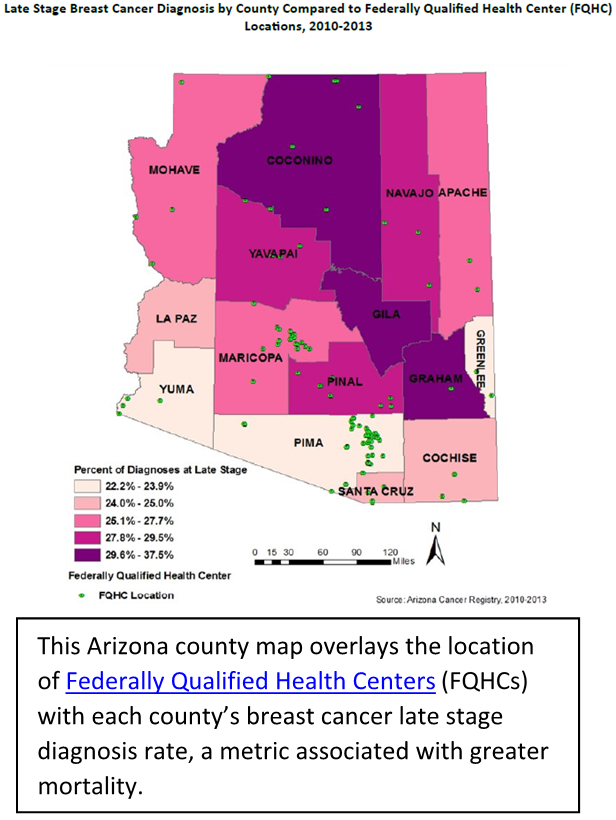 Working with multi-sectoral partners allowed learning community states to change their approaches to breast cancer screening to reach more underserved women statewide. For example, after learning that minority women are diagnosed with breast cancer, on average, seven years younger than non-Hispanic white women, Arizona required mammography providers contracted with the state’s Well Woman HealthCheck screening program to provide free mammograms to qualifying women starting at age 40.
Working with multi-sectoral partners allowed learning community states to change their approaches to breast cancer screening to reach more underserved women statewide. For example, after learning that minority women are diagnosed with breast cancer, on average, seven years younger than non-Hispanic white women, Arizona required mammography providers contracted with the state’s Well Woman HealthCheck screening program to provide free mammograms to qualifying women starting at age 40.
Many states are also exploring telemedicine interventions, such as Project ECHO, a virtual telementoring program designed to reduce health disparities by increasing clinical capacity and improving medical specialization in underserved communities. As a result of the ASTHO learning community, West Virginia founded a Project ECHO site with researchers and administrators at the Charleston Area Medical Center to engage rural primary care providers and improve primary care for breast cancer survivors in areas with poor healthcare access. This initiative is a significant element of West Virginia’s action plan to improve healthcare access and quality for rural West Virginians diagnosed with breast cancer, and represents a strong partnership with a local medical center that was created as a result of the learning community.
Best Practice #4: Implement Evidence-Based Interventions and Promising Practices to Reduce Identified Disparities
There are several resources states can use to learn about evidence-based strategies for addressing breast cancer disparities and improving screening, follow-up after abnormal screening, and treatment quality. The CDC’s Community Guide recommendations, the National Cancer Institute’s database of research-tested intervention programs, and ASTHO’s evidence-based change package contain more information on these approaches and best practices. These resources can be found in the Recommendations section of ASTHO’s online toolkit.
ASTHO’s breast cancer online toolkit provides resources on identifying, measuring, and addressing breast cancer disparities, as well as lessons learned from ASTHO’s Breast Cancer Learning Community. For more information on the learning community, view slides and a recording from the Aug. 8, 2017 webinar, “Reducing Breast Cancer Disparities at the State Level: Promising Practices from the ASTHO Breast Cancer Learning Community,” and visit the ASTHO breast cancer disparities web page.